Case 8
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 65 year old male is presented to OPD with chief complaints of fever and cough since 15 days and shortness of breath since 1 week.
HISTORY OF PRESENT ILLNESS-:
Daily routine(6 years back)
He used to wake up by 7am and was done with his breakfast by 9am then he used to feed his cattle and used to eat whenever he feels hungry and sleep at night by 9pm.
Daily routine(presently)
The Patient wakes up around 8 am and is done with his breakfast by 9am then he used to walk around in the house because he is not able to do any work properly due to blurring of vision, he will have his lunch by 1pm and dinner by 9pm then he used to take his medicines as the Patient said that he is not able to sleep without taking that medicines- Escitalopram and olanzepine.
Patient was apparently alright 6 years back then he developed instability in moods which was observed by his family members and they went to nearby hospital where doctor suggested CT scan and he was diagnosed with lacunar infarct in right thalamus and was on medication, again after 1 year he went for CT scan and he was diagnosed with small hypodense area seen in the right side of the thalamus.
After 3 years he was diagnosed with small hypodense area seen in the both thalamii and he also developed blurring of vision and undergone surgery of left eye due to which he lost his left eye vision completely and had blurring of vision in the right side.
He was admitted here 3 days back with chief complaint of fever and cough since 15 days and shortness of breath since 1 week.
HISTORY OF PAST ILLNESS-:
No history of hypertension, diabetes, asthma, tuberculosis
Patient is on medication-Escitalopram and olanzepine since 2 years.
PERSONAL HISTORY-:
The patient has loss of appetite
Sleep- inadequate
Diet- mixed
Addictions- no
FAMILY HISTORY
There is no similar complaints in the family members.
TREATMENT HISTORY
Patient is on medication due to bordered personality disorder.
GENRAL EXAMINATION
Patient is conscious,coherent and not co-operative at all.
There is no sign of icterus, cyanosis, clubbing, generalised lymphadenopathy.
VITALS :
Temp :febrile
Pulse rate:112bpm
Respiratory rate:22cpm
Bp:110/90 mm/hg
Spo2-98%
GRBS-110mg/dl
SYSTEMIC EXAMINATION:
CVS :
No thrills
No cardiac murmurs
Cardiac sounds-S1,S2 heard
RESPIRATORY SYSTEM :
INSPECTION
PALPATION
PERCUSSION
ASCULTATION
ABDOMEN:
Shape of abdomen-scaphoid
No tenderness
No palpable mass
Hernial orifices-normal
No free fluid
No bruits
Liver ,spleen-not palpable
Bowel sounds -yes
CNS:
Conscious
speech is not proper
No neck stiffness
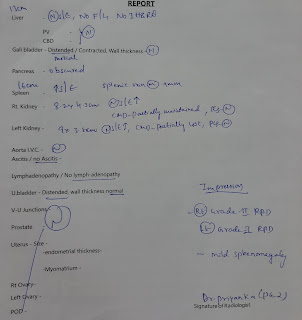
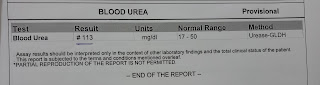
INVESTIGATION
23rd Nov
24th Nov
26th Nov
Diagnosis- Pneumonia with Pancytopenia
Acute kidney injury
Anemia
TREATMENT
22nd Nov
O2 supplementation if spo2<90%
Inj. Neomol 100ml/IV if temp>101degreeF
Tab dolo 650mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Inj Pan 40mg /IV/OD
Fever chart-4th hourly
Vital monitoring- hourly
23rd Nov
O2 supplementation if spo2<90%
Inj. Neomol 100ml/IV if temp>101degreeF
Tab dolo 650mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Inj Pan 40mg /IV/OD
Fever chart-4th hourly
Vital monitoring- hourly
W/f bleeding manifestation
Inj ceftrioxone 1g IV/BD
24th Nov
O2 supplementation if spo2<90%
Tab dolo 650mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Inj Pan 40mg /IV/OD
Fever chart-4th hourly
Vital monitoring- hourly
Inj ceftrioxone 1g/IV/BD
Tab Azithromycin 500mg/PO/OD
25th Nov
O2 supplementation if spo2<90%
Tab dolo 500mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Inj Pan 40mg /IV/OD
Fever chart-4th hourly
Vital monitoring- 2nd hourly
Tab Azithromycin 500mg/PO/OD
Tab olzic 5mg
26th Nov
Tab dolo 500mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Inj Pan 40mg /IV/OD
Fever chart-4th hourly
Vital monitoring- 2nd hourly
Tab Azithromycin 500mg/PO/OD
Tab olzic 5mg
27th Nov
Inj Augmentin 1.2gm
Tab dolo 500mg /PO/BD
Syp Ascoryl 10ml /PO/BD
Neb with pravent and budecort
Tab pan 40mg PO/OD
Tab pragabaliw 75mg PO
Fever chart-4th hourly
Tab Azithromycin 500mg/PO/OD
Tab olzic 5mg
Inform SOS































Comments
Post a Comment