Case 10
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 50 year old female is presented to OPD with chief complaints of shortness of breath, facial puffiness and bilateral pedal edema since 20 days.
HISTORY OF PRESENT ILLNESS-:
Daily routine(before illness)
She used to wake up by 6am and was done with her household work by 7am then she used to go to field for work then returned by 1pm and had her lunch then she used to take rest and had her her dinner by 8pm and sleep by 10pm.
Daily routine(after illness)
She used to wake up by 7am and had her breakfast by 8am and no more go to field for work and just used to do household work and had her lunch by 2 pm and dinner by 9pm then sleep at 10pm after taking medication.
Patient was apparently asymptomatic 1 year back then she developed facial puffiness, swelling in the legs and shortness of breath then she visited nearby local hospital and was diagnosed with chronic kidney disease and was on continuous medication since 1 year.
She came to OPD with chief complaints of shortness of breath at midnight during a walk or when patient sleep in prone position since 1 month and 4 days back she visited hospital and undergone some tests and went back home again as there was no bed available in the hospital then she was admitted yesterday around 12pm and dialysis was suggested according to recent reports.
HISTORY OF PAST ILLNESS-:
Patient is hypertensive since 1 year.
Patient has history of hyperthyroid since 1 year.
No history of diabetes, tuberculosis, epilepsy.
Patient has no history of drug allergies.
PERSONAL HISTORY-:
Diet-mixed
Appetite-lost
Bowel and bladder movement-normal
Micrurition-normal
Sleep-inadequate
No addictions
FAMILY HISTORY-:
No member in the family has similar complaints.
TREATMENT HISTORY-:
Patient has no history of surgical procedure.
Patient is on medication due to chronic kidney injury.
GENERAL EXAMINATION-:
Patient is conscious,coherent and cooperative.
There is sign of pallor.
There is no sign of icterus, cyanosis, clubbing, generalised lymphadenopathy.
VITALS :
Temp :febrile
Pulse rate:99bpm
Respiratory rate:18cpm
Bp:110/80 mm/hg
Spo2-99%
GRBS-115mg/dl
SYSTEMIC EXAMINATION:
CVS :
No thrills
No cardiac murmurs
Cardiac sounds-S1, S2 heard
RESPIRATORY SYSTEM :
Dysponea is present
No wheeze
Position of trachea-central
Breath sounds-vesicular
ABDOMEN:
Shape of abdomen-scaphoid
No tenderness
No palpable mass
Hernial orifices-normal
No free fluid
Bruits present
Liver, spleen-not palpable
Bowel sounds -yes
CNS:
Conscious
Normal speech
No neck stiffness
No kernings signs
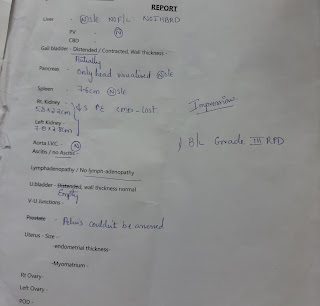
INVESTIGATION-:
Provisional diagnosis-
Chronic kidney disease since 1 year.
Hypothyroid since 1 year.
Anemia
TREATMENT
Fluid restriction<1 lit/day
Salt restriction<2.4gm/day
Tab lasix 40mg PO/BD
Tab nicardia 20mg PO/BD
Tab nodosis 550mg PO/BD
Tab shelcal 500mg PO/OD
Inj erythropoietin 4000 IU
Inj iron sucrose 1 AMP in 100ml
Tab thyronorm 25mg PO/BD



















Comments
Post a Comment