Case 7
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 44 year male is presented to OPD with chief complaints of pain at arterial region of chest region, shortness of breath,bilateral pedal edema,decreased urin output since 10 days.
HISTORY OF PRESENT ILLNESS
Daily routine of patient-:
The Patient is farmer by occupation who wakes up at 7am and is done with his breakfast by 9am then he goes to the field and does farming, he will have his lunch by 1pm and return home from field by 4pm then he used to relax and have his dinner by 9pm and sleep by 10pm-11pm.
Patient was apparently alright 10 days back then he develop sudden pain below the chest during night time.
Patient developed fever associated with chills 1 week back and was admitted in the nearest private hospital where he was diagnosed with typhoid and was treated there.
Patient complaints of bilateral pedal edema(pitting type) upto knee, facial puffiness, loss of appetite, decreased urin output.
HISTORY OF PAST ILLNESS
The Patient is a known case of diabetes and hypertension since 5 year.
No history of epilepsy, asthma, tuberculosis
PERSONAL HISTORY
Patient has loss of appetite
Diet-mixed
Sleep- adequate
Addiction-No
FAMILY HISTORY
There is no similar complaint in the family members.
TREATMENT HISTORY
Patient is on medication due to kidney problem.
GENRAL EXAMINATION
Patient is conscious,coherent, co-operative and well oriented to time and place
There is no sign of icterus, cyanosis, clubbing,lymphadenopathy.
Bilateral pedal edema is present(pitting type)
VITALS
Temperature-febrile
Pulse rate - /min
Respiratory rate-/min
BP-100/50
SPO2-99%
SYSTEMIC EXAMINATION
Thrills-No
Cardiac sound-S1,S2
Cardiac murmer-No
RESPIRATORY SYSTEM
Dyspnoea-No
Wheeze-No
Position of trachea-Central
Breath sounds-Vesicular
ABDOMEN
Shape of abdomen-scaphoid
No tenderness
No palpable mass
No Free fluid
No bruits
Liver and spleen- not palpable
Bowel sound-yes
CENTRAL NERVOUS SYSTEM
Patient is conscious
Speech-normal
Motor and sensory system-Normal
PROVISIONAL DIAGNOSIS
Heart failure
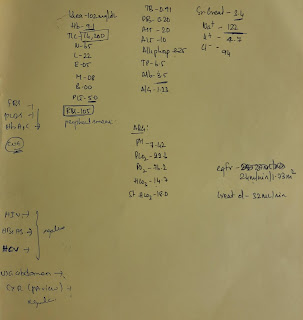
INVESTIGATION-:
TREATMENT
Day -1
-salt restriction <2.4gm/day
-fluid restriction <1lit /day
-Tab TELMA AM /PO /OD
-Inj LASIX 40 mg IV/BD (if BP >110mg/hg )
-Inj PANTOP 40 mg IV/BD
-Tab NODOSIS 550mg PO/OD
-Tab SHELLAC 500mg PO/OD
-Tab PLM 500 mg PO /SOS
-Inj NEOMOL 100 ml /IV/SOS (if temp .>101degreeF )
-Temp charting 4th hrly
-Inj PIPTAL 4.5gm IV /BD
Day-2
salt restriction <2.4gm/day
-fluid restriction <1lit /day
-Tab TELMA AM /PO /OD
-Inj LASIX 40 mg IV/BD (if BP >110mg/hg )
-Inj PANTOP 40 mg IV/BD
-Tab NODOSIS 550mg PO/OD
-Tab SHELLAC 500mg PO/OD
-Tab PLM 500 mg PO /SOS
-Inj NEOMOL 100 ml /IV/SOS (if temp .>101degreeF )
-Temp charting 4th hrly
-Inj PIPTAL 4.5gm IV /BD
-Inj hai pxemeal s/c





















Comments
Post a Comment