Case 5
This is an online e-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
A 45 year old male presented to OPD with chief complaints of fever and chills since 4 days.
HISTORY OF PRESENT ILLNESS
Patient was apparently alright 4 days back then he develope muscle cramps and cough initially
No history of chest pain, pedal edema,blurring of vision,loose stool.
HISTORY OF PAST ILLNESS
No history of diabetes, asthma, CAD, hypertension, tuberculosis, previous surgery
PERSONAL HISTORY
Diet-Mixed
Appetite-Normal
Bowels-regular
Sleep-normal
FAMILY HISTORY
No history of hypertension, diabetes, heart disease, asthma,cancer, tuberculosis
GENRAL EXAMINATION
Patient is conscious,coherent, co-operative and well oriented to time and place
There is no sign of pallor,oedema of left foot
There is no sign of cynosis,lymphadenopathy
VITALS
Temperature-febrile
Pulse rate - 70/min
Respiratory rate-18/min
BP-130/90
SPO2-99%
SYSTEMIC EXAMINATION
Thrills-No
Cardiac sound-S1,S2
Cardiac murmer-No
RESPIRATORY SYSTEM
Dyspnoea-No
Wheeze-No
Position of trachea-Central
Breath sounds-Vesicular
ABDOMEN
Shape of abdomen-scaphoid
No tenderness
No palpable mass
No Free fluid
No bruits
Liver and spleen- not palpable
Bowel sound-yes
CENTRAL NERVOUS SYSTEM
Patient is conscious
Speech-normal
Motor and sensory system-Normal
PROVISIONAL DIAGNOSIS
Viral Pyrexia with thrombocytopenia
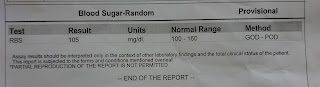
INVESTIGATION
26th October
27th October
TREATMENT
TREATMENT GIVEN:
-Inj TAXIM 1G IV/BD
-IVF-NS, RL @100ml /hr
-Inj PAN 40 mg PO/OD
-Inj OPTINEURON 1amp in 100 ml NS/IV/OD
-Tab PCM 650 mg PO/BD
-strict I/O charting
-Temp,BP,PR monitoring
-plenty of oral fluids













Comments
Post a Comment